Blind Patient Regains Vision Following Cortical Implant: Unexpected Discovery Challenges Understanding of Optic Nerve Recovery
 A Spanish research team has documented an extraordinary case of vision restoration in a patient who had been completely blind for nearly four years due to bilateral optic nerve damage, a finding that may reshape thinking about neural regeneration and rehabilitation strategies.
A Spanish research team has documented an extraordinary case of vision restoration in a patient who had been completely blind for nearly four years due to bilateral optic nerve damage, a finding that may reshape thinking about neural regeneration and rehabilitation strategies.
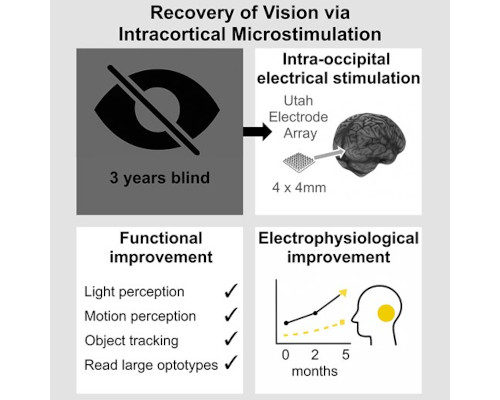
The 65-year-old man, who lost all vision following bilateral non-arteritic anterior ischaemic optic neuropathy (NAION) in 2018, unexpectedly regained functional sight after receiving an intracortical microelectrode array as part of a visual prosthesis trial at the University Miguel Hernández in Spain.
Within two days of the implant surgery, the patient began perceiving lights and movement. By six months, his visual acuity had improved 23-fold binocularly, enabling him to read large characters and navigate independently—capabilities that persisted even after the device was surgically removed.
An Unintended Outcome
The case, published in Brain Communications this month, represents the first documented instance of spontaneous vision recovery following cortical electrical stimulation in a patient with complete blindness lasting more than three years.
"This recovery allowed him to perceive light, motion and even read large characters," wrote lead author Dr Eduardo Fernandez and colleagues. "Although our results are based on a single case, they could contribute to the development of new therapeutic approaches and rehabilitation paradigms for individuals with damage to the optic nerve in the future."
The research team emphasised that the electrical stimulation protocol was designed to elicit artificial visual percepts, not to restore natural vision. Among four trial participants tested, this patient was the only one to experience measurable improvement in natural visual acuity.
Exceptional Timeline for NAION Recovery
The timing of the recovery challenges conventional understanding of NAION prognosis. While spontaneous improvement occurs in up to 42.7% of NAION patients, this typically happens within the first few weeks and rarely extends beyond 2–3 months post-injury.
In this case, vision restoration began 3 years and 10 months after the initial bilateral damage, an unprecedented timeframe.
Prior to surgery, the patient had no light perception in either eye, bilateral mydriatic pupils with minimal response to light in the left eye only, and pallid optic nerves consistent with bilateral optic atrophy. Visual evoked potentials were nearly undetectable.
Measurable Improvements Documented
The research team used standardised low-vision assessment tools to track the patient's progress:
- Basic Assessment of Light and Motion (BaLM): Ceiling performance achieved within one week post-surgery across all modules (light perception, temporal resolution, light location, motion direction)
- Freiburg Acuity and Contrast Test (FrACT): Progressive improvement throughout the six-month experimental period, with maintained gains at follow-up
- Visual Evoked Potentials: Left eye showed increased P1 amplitudes and eventual normalisation of latencies; right eye remained more impaired but above baseline
Eighteen months after device explantation, binocular vision remained 11 times better than pre-implantation levels, despite some decline over time, particularly in the right eye.
Possible Mechanisms Under Investigation
The researchers propose several potential explanations for the unexpected recovery:
- Neurotrophic-like effects: Chronic intracortical microstimulation may trigger molecular cascades analogous to endogenous neurotrophic factors, promoting synaptic sprouting and neuronal health—similar to effects observed with retinal prostheses.
- Activity-dependent regeneration: Animal studies suggest postsynaptic neuronal activity plays a critical role in promoting retinal axon regeneration. The electrical stimulation may have initiated similar processes in residual neural pathways.
- Unmasking of latent circuits: Intensive visual training combined with electrical stimulation could have enhanced function in partially injured pathways, reducing intracortical inhibition and reopening adult visual cortical plasticity.
- Preservation of minimal substrate: Unlike other trial participants, this patient retained minimal pupillary response in one eye pre-surgery, suggesting a critical threshold of viable neurons may be necessary for recovery.
Clinical Implications
The findings raise important questions about rehabilitation approaches for optic nerve damage. The research team noted that visual training and patient motivation likely played significant roles alongside the electrical stimulation.
"Training is the most commonly used strategy to modulate visual plasticity and support visual recovery," the authors wrote. "The combined effects of intensive, attention-driven visual training and electrical microstimulation could contribute to enhancing function in partially injured pathways."
However, the researchers cautioned that this represents a single case, and outcomes may vary significantly depending on visual pathology, residual vision, and duration of blindness.
Broader Research Context
The case emerged from an ongoing clinical trial (NCT02983370) investigating the feasibility of Utah Electrode Array technology for cortical visual prostheses in profoundly blind individuals. The trial focuses on understanding optimal stimulation parameters, long-term tissue responses, and individual variability in brain structure and function.
While no cortical visual prosthesis is currently available for clinical use, multiple research groups worldwide are pursuing various approaches to restore functional vision through direct cortical stimulation.
The Spanish team acknowledged that their stimulation protocol was not designed as a therapeutic intervention, and patients were informed no short- or long-term benefit was expected. The primary aim was to generate knowledge for future prosthesis development.
What This Means for Practitioners
For eyecare professionals, this case highlights several considerations:
- The potential for neural recovery may extend far beyond currently understood timeframes
- Residual neural function, even minimal pupillary responses, may indicate rehabilitation potential
- Combined approaches involving electrical stimulation and intensive visual training warrant further investigation
- Current prognostic frameworks for NAION may need revision
The researchers emphasised that future studies must determine whether this represents an isolated event or indicates reproducible mechanisms that could inform new treatment strategies.